Psoriatic Arthritis or Osteoarthritis?
Introduction
Many patients with psoriasis report joint pain. If a doctor treating the psoriasis records joint pain then psoriatic arthritis (PsA) is a possibility. This could lead to the use of powerful drugs which may not work if the pain is coming from osteoarthritis (OA). This page explains why it can be hard to tell OA or "wear and tear" from PsA and how to deal with this problem.
Overlapping features of OA and PsA
Both OA and PsA most commonly begin after the age of 40. Both are associated with increased body weight and both may be linked to preceding joint injury.
Although OA is known as a disease of "wear and tear", there is lots of inflammation in the joints especially in the early stages of disease and this is known as inflammatory OA [1]. Accordingly, if OA comes to attention in this fashion it may be associated with cardinal features of PsA that includes joint stiffness and swelling.
Because OA and psoriasis are so common there is a danger of making an incorrect diagnosis of PsA in a subject with OA and psoriasis. Psoriasis affects up to 2% of the population and given that OA is very common, these two conditions may co-exist. As Dr Hickam famously put it; "a man can have as many diseases as he damn well pleases". This is known as "Hickam's dictum" and means that both psoriasis and OA can be present at the same time.
Overlap in joint Distribution of OA and PsA
The generalised form of OA that affects the hands involves the DIP and PIP joints of the hands. It also typically involves the spine including the cervical spine (neck) and lumbar spine (low back). These are also common site for PsA spinal involvement.
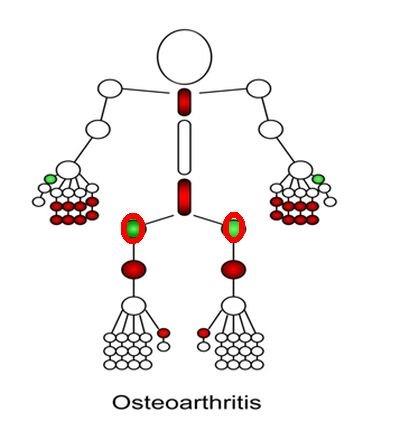
|
| Typically generalised nodal OA involves the joints shown in the following graphic which include the small joints of the hand and joints and spine, both of which are generally spared in OA. Apart from the big toe the other toe joints are spared. |
The generalised pattern of OA is commoner in women than in men and this should arouse suspicion. The 2nd to 5th toes are more likely to be involved in PsA and may show sausage digits. However, these joints are usually spared in OA.
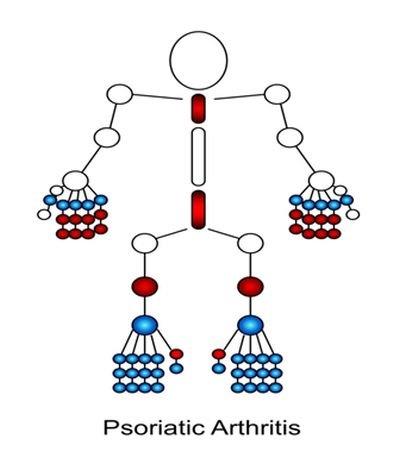
|
| As can be seen in this cartoon the distribution of PsA can be remarkably similar to OA Small joint involvement of the toes more likely in PsA as is sausage digits. Nail and scalp psoriasis may also favour PsA as a diagnosis in a patient with joint pain, but this is not proven beyond doubt. |
Complicating factors
In addition to the common anatomical patterns of disease it is also possible that PsA will trigger secondary OA. Put another way, the inflammation can trigger secondary "wear and tear".
Osteoarthritis may start with an small joint swelling that looks like PsA. Only later does this give rise to the characteristic OA related changes of Heberdens or Bouchards nodes which point to OA as the correct diagnosis [2]. This could take several years to develop.
Tools of the trade to distinguish OA and PsA
Non-steroid inflammatory drugs may help both groups but might be slightly better in PsA.
A corticosteroid injection may also be temporarily effective for both PsA and OA. However, in a patient with extensive psoriasis or a history of extensive psoriasis this could lead to a severe skin disease flare.
When in doubt the selection of drugs to treat the skin should also consider ones that treat arthritis.
References

