Achilles enthesitis as an unrecognised cause of heel pain in the seronegative spondyloarothpathies and psoriatic arthritis
Introduction
The Achilles enthesis takes its name from the ill fated Greek hero of the same name.
 |
| This is a statue of The dying Achilles by Ernst Herter from the Achilleion in Corfu. The most famous enthesis of all- The Achilles insertion is named after him. It is the premier enthesis and is located in the foot |
In general enthesitis is more common in the lower limbs compared to the upper limbs.
It also involves larger entheses e.g. Achilles tendon insertion more often than smaller ones.
 |
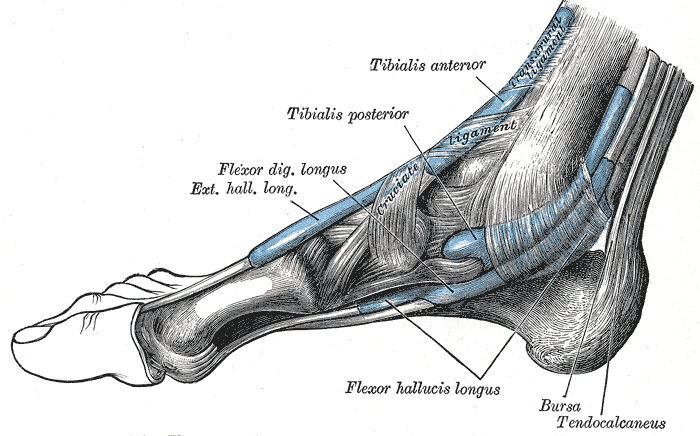 |
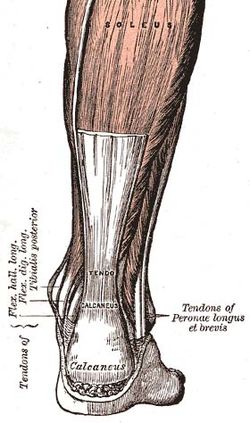
| The Achilles enthesis is a major insertion in the foot. It forms an elaborate enthesis organ. It is attached to the calcaneus over a wide area. | |
The heel is reported to be the most common site of enthesitis related foot pain [1, 2].
However there are other important "functional entheses" in the foot including where tendons wrap around bones that can also cause foot pain.
Heel and foot pain represent common reasons for referral into podiatry and physiotherapy services.
The diagnosis of spondyloarthropathy including Ankylosing Spondylitis, Psoriatic Arthritis and other Spondyloarthropathies may be missed if the symptoms are confined to the heel.
The failure to recognise inflammatory enthesitis may lead to a delay in diagnosis or even incorrect treatment including surgery.
Recognition of Achilles enthesitis
Achilles Enthesitis or primary inflammation of the insertion is associated with early morning stiffness of the insertion and pain.
This usually improves as the day goes on.
There are no obvious aggravating features such as sporting activity.
The role of injury or trauma as a trigger for enthesitis is still unclear.
Severe enthesitis may be painful and lead to limping throughout the day.
On clinical examination there may be tenderness and swelling at the insertion.
On clinical examination there may be tenderness only without swelling.
Some cases manifest as swelling of the retrocalcaneal bursa that is part of the Achilles tendon synovio-entheseal complex.
If enthesitis is severe there may also be swelling of the adjacent tendon.
X-rays may show new bone formation or erosion of the insertions.
Isolated enthesitis of the heel can be incredibly disabling.
Diagnosis of Achilles enthesitis
The diagnosis is based primarily on the history and physical findings.
X-rays may be normal in early disease.
Ultrasound may show inflammatory changes in the enthesis organ.
Magnetic Resonance Imaging may also show soft tissue changes and diffuse bone marrow involvement in the adjacent bone.
Key point - the imaging appearances of different pathologies that afflict the Achilles can look remarkably similar. Physicians need to carefully evaluate imaging reports in the context of the history and clinical findings.
Treatment of Achilles enthesitis
Correct foot malalignment where present
Heel supports to minimise trauma and to lessen stretch on Achilles may be tried.
Physiotherapy stretching exercises to loosen tight Achilles tendons to take strain of enthesis.
Anti-inflammatory drugs often work for milder or self-limiting disease.
The role of drugs such as methotrexate or sulphasalasine for isolated enthesitis is presently dubious
Resistant cases may respond well to anti-TNF [4].
As an alternative local injection of anti-TNF therapy may also work but the role of such strategies over cheaper options including steroids is unclear [5].
For really difficult cases there is evidence that switching to a second anti-TNF drug may help [6].
Other common causes of Achilles tendon region pain
Enthesitis may be misdiagnosed as the following conditions
- Degenerative enthesopathy- This usually occurs in older subjects and tissue swelling is 2.5 cms away from the enthesis.
- Haglunds Deformity- This painful condition of the Achilles tendon synovio-entheseal complex region.
- Achilles tendonitis that typically occurs in active runners or sports activists.
This represents a mixed bag of pathologies that includes:
- Achilles tendon thickening or degeneration
- Inflammation of the tissue adjacent to the tendon or paratenon,
- Over prominence of the tuberosity
- Retrocalcanceal bursa and adjacent fat thickening or inflammation
- New bone formation at the enthesis
For the most resistant cases there is evidence that surgery may help this group of cases [1, 2]. However it is essential to establish the correct diagnosis.
The MRI appearances of classical Achilles tendon injuries are shown below
 |
 |
| When the Achilles fails it usually fails within the tendon proper (left panel) or is associated with failure in the underlying bone due to a stress fracture (right panel). The failure in the bone is due to the strong functional integration between the insertion and the bone. The right panel also shows fluid in the adjacent retrocalcaneal bursa as this is also a functional part of the enthesis [image courtesy of Radzone]. | |
Illustrative case. Inflammatory enthesitis misdiagnosed as Haglund deformity
A 24 year old nurse presented with a one year history of chronic heel pain.
She had severe joint stiffness throughout the day.
Her left heel was tender and swollen over the Achilles insertion, adjacent tendon and bursa.
She was sent to a podiatrist who referred her to an orthopaedic surgeon.
She was diagnosed as having severe Haglunds deformity and was offered surgery.
She declined this and sought a second opinion with a Rheumatologist.
She was not an active sports participant that is typically seen in Haglunds deformity.
She was noted to have inflammatory sounding enthesitis. She had no evidence of psoriasis.
Bulbous swelling of the Achilles insertion and adjacent bursa was noted.
Her CRP was marginally elevated and she was HLA-B27 positive.
A diagnosis of isolated HLA-B27 associated inflammatory enthesitis was made.
Due to extreme disability she was treated with etanercept and within 3 months had return of normal function.
Note 1 - In the UK patients with resistant isolated enthesitis do not meet the NICE criteria for the use of anti-TNF therapy for isolated enthesitis in spondyloarthropathy. However, the only compelling evidence for the therapy of resistant heel enthesitis comes from the anti-TNF class of drugs [5]
References



