Distal Interphalangeal Joint Disease in Psoriatic Arthritis
Introduction
The distal interphalangeal joints (DIPs) are those joints adjacent to the nails. These are a characteristic site of involvement in Psoriatic Arthritis (PsA) [1].
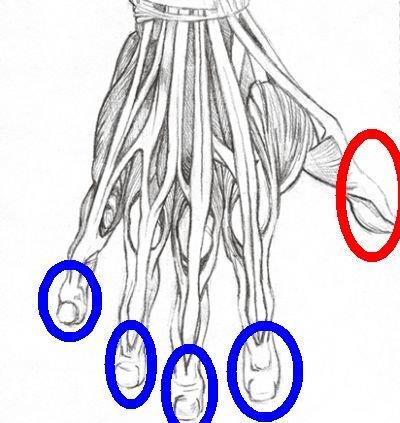
|
| This drawing shows the distal interphalangeal joints (DIPs ) of the fingers inside the blue circles. The thumb has one less joint than the fingers and the joint adjacent to the nail is called the interphalangeal (IP) joint. |
DIP Joint Disease Facts
The DIP has a joint cavity lining (termed synovium). Rheumatoid Arthritis (RA) attacks synovial joints but this joint is usually spared in RA. The reason for this remains unknown. In a patient with multiple swollen joints that includes DIP swelling then an alternative diagnosis to RA is nearly always the case.
In PsA diffuse swelling of the joint may be evident. When the joint is scanned with high powered magnetic resonance imaging (MRI), inflammation of the mini-entheses around the joint is very common [2]. These entheses include the joint stabilisers called the lateral collateral ligaments, the extensor and flexor tendons.
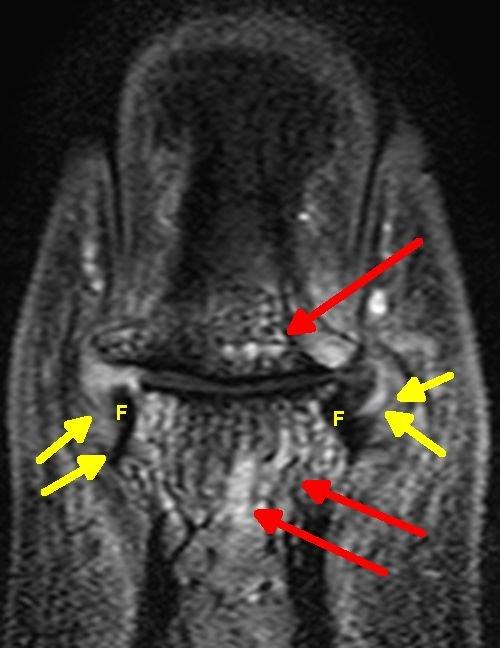
|
| This is an MRI scan of acute PsA of the DIP joint. The red arrows show diffuse bone inflammation which is linked to enthesitis. The yellow arrows show the entheses of the collateral ligaments which are inflamed. The letter F denotes the fibrocartilage at the ligament attachment sites. The fibrocartilage has no blood vessels and tends to escape the earliest inflammatory lesions. |
DIP Disease Mechanism
Remarkably all of these tendons don't just anchor the bones together but also anchor the nail directly to the bone. This explains the strong link between nail disease and DIP joint inflammation [1]. Nail disease can also been seen with arthritis in other joints at sites well away from the DIP but this is less common.
This joint is subject to lots of stress related to supporting the body weight, lifting heavy objects, minor injuries and related to the fact the nail is anchored directly to it. Collectively these factors probably play a role in disease localisation to that site.
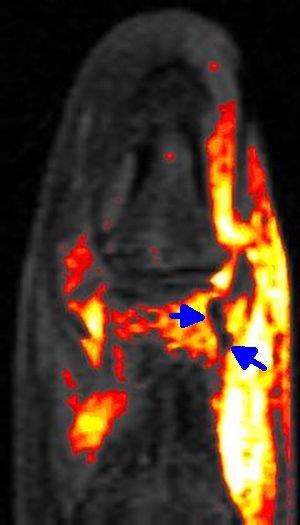
|
| This is a contrast enhanced image of a different case showing severe inflammation of the DIP joint in early PsA. The blue arrows show the stress resisting fibrocartilage which has no blood vessels and as spared in the acute phase. With disease persistence these shock absorbing tissues can get eaten away by the inflammation. |
DIP joint involvement is usually part of a more generalised form of PsA. On occasion DIP arthritis of many joints is evident or DIP arthritis confined to one or two joints but this is fairly rare. The greatest utility of clinical DIP disease is that it helps distinguish a polyarthritis from RA where these joints are spared.
The DIP joint is the commonest location for a pattern of PsA called arthritis mutilans. Fortunately, this seems to be rare in the modern era.
Pitfalls
Distinguishing PsA from Osteoarthritis of the DIP can be very difficult. Even with high quality MRI scanning it can be impossible to tell these two conditions apart.
References

