Back pain and Normal MRI scan in AS
Introduction
Patients with symptoms that are classical of Ankylosing Spondylitis (AS) may have a normal MRI scan that is "not showing any inflammation". This is despite the fact that an X-ray may have previously shown sacroiliitis and the patient may have on-going sacroiliac joint pain and stiffness or similar symptoms elsewhere in the spine.
If a patient has confirmed sacroiliitis and then develops severe spinal pain they may be perplexed to hear that an MRI of the spine is normal and that there is "nothing wrong". This page explains how diseases of spinal entheses can be difficult to visualise and accounts for these apparently normal scans.
Explanation for Normal MRI and back pain in AS
In the spine the pain in AS is invariably coming from the entheses and adjacent bone. The spinal inflammation in AS is really a multi-site enthesitis or poly-enthesitis as shown in the figure below.
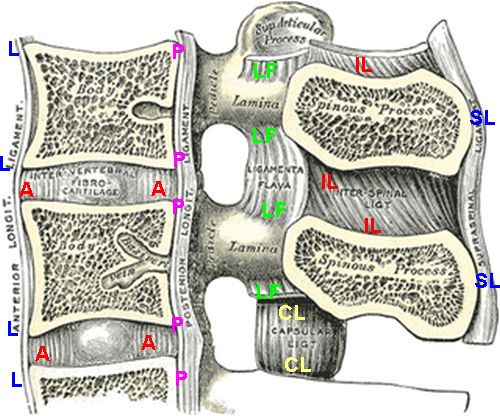
|
| There are multiple entheses in the spine which are marked in this cartoon that shows on
3 of over 20 vertebrae.
A = annulus fibrosus (disc)
L = anterior longitudinal ligament
P = posterior longitudinal ligament
LF = ligamentum flavum
CL =capsular ligament (at facet joints)
IL = interspinous ligaments
SL =supraspinal ligaments
Several other entheses not shown. Spinal inflammation in AS is due to multiple sites of
enthesitis and adjacent osteitis (bone inflammation)
|
Tissue basis for Normal MRI appearance
The normal enthesis is subject to high levels of mechanical stressing. The normal enthesis has fibrocartilage at attachment sites and has no blood vessels. The ligament or tendon of an enthesis has comparatively few blood vessels but have lots of nerve endings. This is reviewed in detail in the Anatomy and Physiology section.
This apparent normality is because the enthesis structure with few, or no blood vessels minimises the magnitude of inflammatory reactions and the MRI scanners we use are not able to visualise these structures clearly.
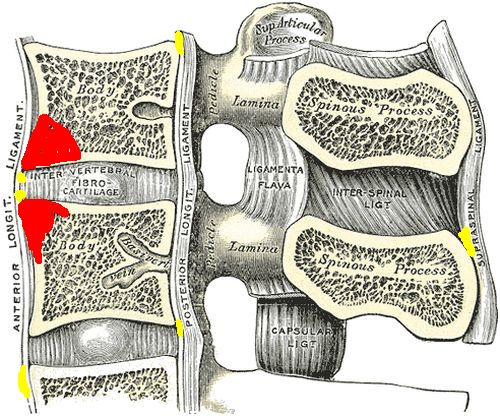
|
Because the soft tissue part of the enthesis is lacks a blood supply and the tissues are tightly knitted together and the structures are small, an MRI may appear normal. This in contributed to by the low resolution of MRI. The subtle degrees of inflammation that are hard to see are shown in yellow. However, the bone at the enthesis attachment sites is very vascular and as a result inflammation over this bigger territory is readily seen on MRI when it is present (this is shown in red) If enthesitis is not associated with inflammation in the underlying bone it may be impossible to see the changes in the soft tissue of the enthesis on MRI. |
The MRI scan is not able to visualise these subtle changes in the soft tissue non-bony part of the enthesis due to the tissue structure of this part of the enthesis. However, the underlying bone is very well supplied with blood vessels and inflammation is easy to appreciate at this site
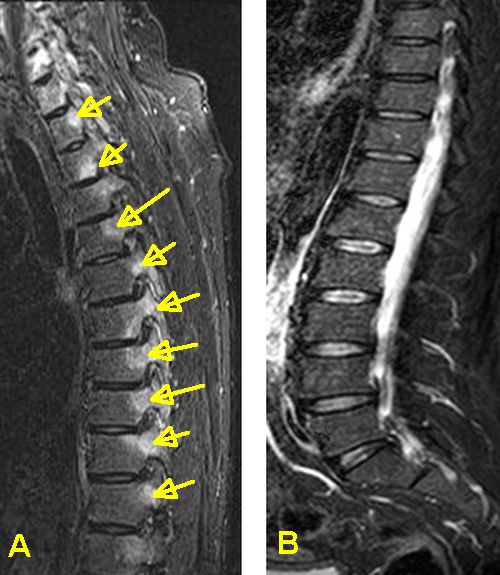
|
These scans are from two patients with spinal enthesitis in AS. Because the first patient developed bone involvement at the enthesis this is readily seen on MRI (yellow arrows) The absence of bone inflammation in the second case points towards the soft tissue parts of the enthesis being involved. This have a much lower blood supply but lots of nerves and are harder to appreciate. |
Tissue studies have also shown bone inflammation where MRI scanning is normal so it is possible that low level inflammation not detected by MRI might cause pain. However, given that normal insertions show micro-inflammation related to stressing it is not clear what exactly the tissue studies of a non-inflamed MRI detected area represent.
Alternative Diagnoses and Implications of Normal MRI scan in AS
A negative MRI of the spine in a patient with AS and back pain does not mean the patient has fibromyalgia. It could still well be inflammatory in nature and may need treatment. Of course the report of a normal MRI in AS raises other possibilities other than on-going inflammation related to AS
Mechanical related pain due to AS related posture change, muscle imbalances or scarring due to chronic established AS can contribute to pain
Degenerative related arthritis including facets joint and disc disease may contribute to pain
However, the absence of bone inflammation on MRI may be a good prognostic sign and might mean that the bones may be less likely to fuse. More research is needed in this area in AS.
Skeletal radiologists looking at MRI scans of the spine will check the adjacent structures including the pelvis to search for alternative causes of pain.
Treatment options for normal MRIs in AS
Patients with established AS can still be treated on the basis of the disease activity score including BASDAI. However, a normal MRI is associated with a lesser response to therapy.
It is more difficult to know what to do in a patient with early inflammatory back pain, who is HLA-B27 positive with a normal X-ray and normal MRI. This is especially the case if such a subject has a relative with AS or has other suspicious features such as uveitis or psoriasis. Without clear evidence for inflammation on MRI or blood tests treatment with biological drugs is not usually undertaken.
Disease progression may be less if the MRI scan shows no changes since positive MRI scans have been linked to spinal fusion progression.
Pitfalls
Between the time the scan is ordered and performed the inflammation may spontaneously go away and return after the scan is performed. A second scan may detect the inflammatory changes where the original scan was normal.
