Different forms of psoriasis and PsA
Introduction
Patients with a minor degree of psoriasis are not generally sent to see a Dermatologist and are managed by the family doctor. In some cases they may not even see a doctor and attribute a scalp problem to dandruff rather than psoriasis. They may attribute psoriatic nail disease to a fungal infection. In the absence of significant psoriasis, the possibility of psoriatic arthritis (PsA) may not be considered and specialist referral may not be made when joint pains develop with these being attributed to age related "wear and tear".
The purpose of this page is to highlight that some types of psoriasis are more linked to enthesopathy and associated joint swelling than other patterns.
Scalp, Nail and Genital Psoriasis predict PsA
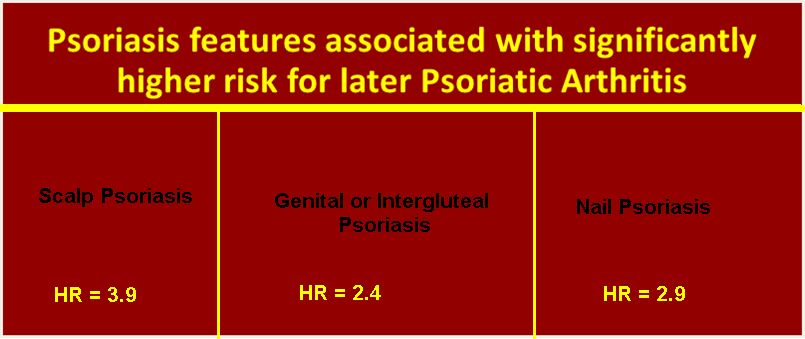
In patients with psoriasis the presence of scalp disease, nail disease or psoriasis in the genital regions are much more likely to PsA development. Young patients with extensive psoriasis without involvement of these sites may be less likely to develop PsA [1].
Generally speaking there is no link between the severity of psoriasis and the severity of skin disease. Most people in hospital for treatment of extensive psoriasis do not have PsA.
|
| This figure is based on work from Wilson and colleagues [1]. It shows that psoriasis in certain parts of the body predict PsA. |
The extensive body psoriasis that young people often get is linked to carriage of a gene called HLA-Cw06. This gene is not shared with PsA and may explain why bad psoriasis is not necessarily linked to arthritis.
Patterns of Psoriasis and Enthesopathy
Thus far nail disease in psoriasis cases has been linked to silent enthesopathy (no pain but visible enthesis abnormalities on scanning) in the lower limbs and adjacent to the nail itself [2].
Studies to link enthesopathy to scalp or genital psoriasis have not been reported to date.
Implications
In people with possible scalp, nail or genital psoriasis who develop joint pain, stiffness and swelling, PsA should be considered.
With joint pains look for nail pits in particular. These are more specific for psoriasis than onycholysis which may also occur with fungal infection.
Consider that dandruff or an itchy scalp in presence of joint pains may be connected to psoriasis
A rash between the buttocks or genital area, although potentially embarrassing, should be brought to attention by patients and looked for by doctors.
References


Resources
http://www.papaa.org/further-information/scalp-psoriasis
http://www.psoriasis.org/about-us/contact
http://www.psoriasisrx.com/Scalp_Psoriasis.asp
http://www.psoriasisrx.com/Nail_Psoriasis.asp