The Nerve Supply of the Enthesis and Pain Mechanisms
Enthesopathies can be very painful but despite this doctors frequently fail to recognise pain emanating from these structures. This page explain why enthesopathies cause pain that may be poorly recognised.
It may be surprising to learn that a normal, healthy fibrocartilaginous enthesis lacks nerve fibres at the hard-soft tissue interface which is a site of very high stressing.
Hence, the enthesis is often described as being 'aneural'.
Cartilages elsewhere, including the articular cartilage that lines the ends of long bones is also aneural. That cartilage in general (and thus enthesis fibrocartilage in particular) lacks a nerve supply must relate to its capacity to withstand compression. The likelihood is that compressive loading would trigger any nerves to fire more or less continuously resulting in chronic pain.
Why is enthesopathy associated with pain if the insertion site lacks nerve endings? This is because the nerves endings are near or adjacent to the insertion site.
Nerve endings may be located on the surface of the attachment site within the loose connective layer that is known as the epitenon.
Nerve endings have also been documented in fat that lies deep to the attachment site - i.e. at the insertional angle. As this fat is compressed when the insertional angle is decreased with joint movement, any nerve fibres between the fat cells are likely to be stimulated.
Some types of nerve endings may sense pain but others sense the joint position in 3D space or what is known as proprioception. It has been suggested therefore that such innervated fat has a proprioceptive role. e.g. the fat known as Kager's fat pad that lies in the insertional angle of the Achilles tendon. So pain and joint position may originate in this structure.
Pain may also originate from the bone underneath insertions especially when there is bone damage or pressure changes within the bone due to disease states.
Therefore pain may originate in several locations near insertions but not from the insertion itself.
When micro damage occurs at insertions then blood vessels may invade the region containing fibrocartilage as part of the normal repair process. However, this process may go wrong with the consequence that blood vessels persist at these sites. It is thought that blood vessels may "piggy back" nerve endings into the insertion site thus leading to persistent pain.
This may then contribute to chronic low back pain in disc degeneration.
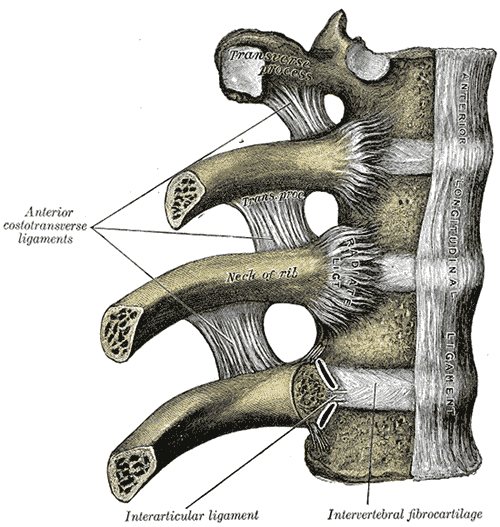 |
| This shows some ligament and capsule attachments that anchor the bones of the spine. The region labelled intervertebral fibrocartilage comprises the capsule that connects vertebrae. In health this structure has no blood vessels at its insertion point but in patients with chronic low back pain blood vessels may invade the fibrocartilage and "piggy back" nerve endings. This leads to pain especially during loading. |
Because of the anatomical structure of the enthesis it tends not to swell up when inflamed. This is the opposite of joint cavity disease where pain and swelling are more likely to occur together. Blood tests and X-rays may be normal in the case of enthesopathies lead to a poor localisation and diagnosis of pain.
Painful enthesopathies may not be recognised especially if the site of involvement is not directly accessible to examination such as spine or chest.
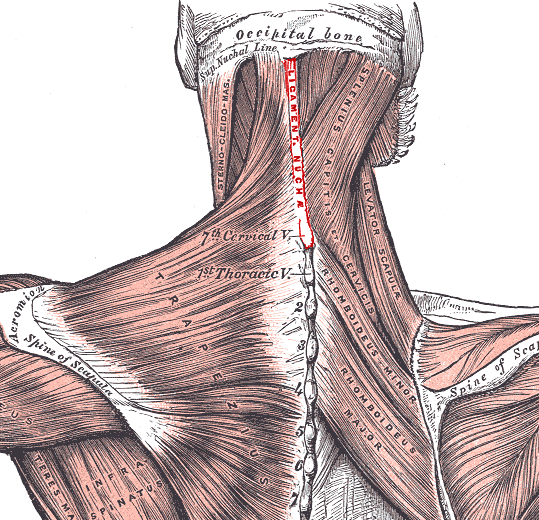 |
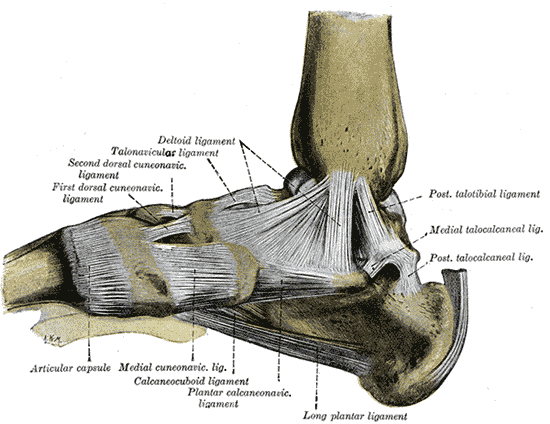 |
| This shows some accessible insertions including those of the neck and spine where enthesopathy can be accurately diagnosed on examination of the attachment sites | This image shows ligaments deep within the foot. The entheses of these ligaments holds the bones together. It can be very difficult or impossible to determine that pain is emanating from these regions since they are deeply located |