New Bone Formation in AS
Introduction
New bone formation is the major cause of permanent disability in Ankylosing Spondylitis (AS). Although new bone formation occurs both in the peripheral and axial (spinal) skeleton, it is the spinal involvement that is strongly associated with disability as it can lead to the 24 mobile vertebrae fusing together to effectively form a solid column of bone.
|
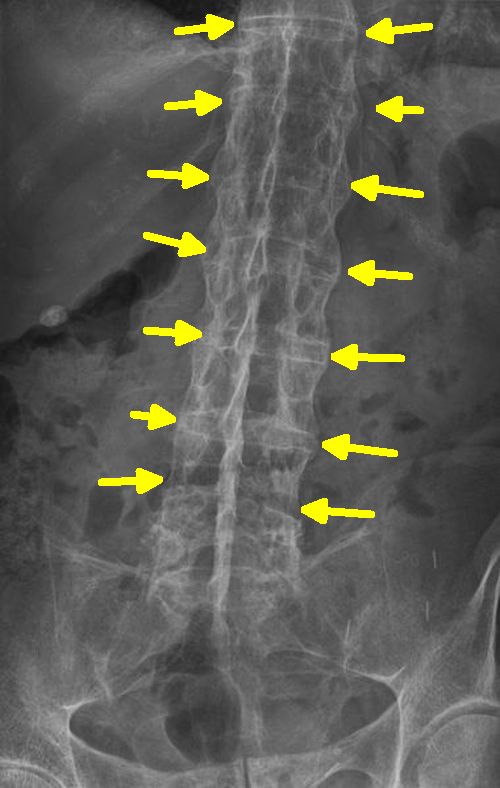
| This is an example of new bone formation with complete fusion of the spine due to new bone formation bridging across the entheses adjacent to the spinal discs (yellow arrows). Modified from Wikipedia |
New Bone Formation Mechanism in AS
In AS it is now evident that there is a strong link between new bone formation and preceding spinal inflammation [1].
Bone formation in AS may be an over exuberant repair response and may follow adjacent bone erosion in some cases. This is the opposite of Rheumatoid Arthritis where erosion leads to progressive joint destruction.
Although several genes and molecules have been defined in AS, the possible genes that can predict new bone formation reliably have not been identified.
A degree of new bone formation may actually occur as an age related phenomenon at normal entheses especially at sites of tension on bone [2]. The reaction taking place after resolution of a bout of entheseal inflammation appears to exaggerate this tendency.
New Bone Formation in the Spine in AS
The best predictors of new bone formation in the spine are
- Radiographic evident new bone at baseline
- Male sex
- Smoking
- High disease activity score e.g. BASDAI
- Elevated inflammatory markers
- "Bone oedema" (US English "edema") which is MRI determined inflammation.
- Possibly Occupations that involve heavy lifting
With progressive AS new bone formation can occur at virtually every enthesis around the spine.
In the spine the disc spaces are not usually obliterated by new bone formation and the new bone formation is around the outside of the disc only. In the sacroiliac joint, the entire joint space may be completely obliterated due to bone fusion. Since the sacroiliac joint moves to only a tiny degree in health the loss of movement may not cause major problems.
New bone formation may also be seen along the large entheses of the pelvis that correspond to large muscle attachment sites.
Therapies and New Bone Formation
The oldest class of drugs to treat AS, which are the non-steroidal anti-inflammatory agents (NSAIDs), may inhibit new bone formation. More research is needed into this aspect of disease.
There is some emerging evidence that the anti-TNF class of drugs eventually slows down the progression of spinal new bone formation in AS. More work is needed to confirm this, especially studies in patients with the earliest phases of disease [3].
Theoretically other classes of biological drugs may slow down new bone formation by hindering bone stimulating molecules called bone morphogenetic proteins (BMPs). This may be the case in experimental models but no data is available in man thus far [4].
Stopping New Bone Formation
The holy grail in AS therapy would be an agent that stops both inflammation and its subsequent new bone formation reaction.
The best predictor of new bone formation is the presence of new bone in the spine. However, with the modern emphasis on seeing cases really early in disease this might require repeated X-ray assessment of the spine. More work is needed in this area.
New bone formation is so variable between patients in its rate of progression that it is very hard to study in clinical trials.
Implications
This is one of the hottest areas of research in AS. The identification of patients that are highly likely to progress to complete spinal fusion would prompt early and more effective therapy.
Conversely, the presence disease limited to the sacroiliac joint, especially mild disease might be used to ensure that therapies could be carefully applied to cases that most need them. This is of vital importance to health economists and payers.
References




Resources
University of Cambridge DoITPoMS Structure and composition of bone Resource on basics of bone formation.
Amgen New Insights Into Bone Biology nice graphics on basic bone biology.