Distinguishing PIP joint OA from PsA
Introduction
The proximal interphalangeal (PIP) joint is commonly involved in Psoriatic Arthritis (PsA). It is also commonly involved in other common types of arthritis including osteoarthritis (OA) and in rheumatoid arthritis (RA). This page explains why it can be difficult or impossible to tell whether PIP swelling is due to OA or PsA. This is because both types of disease involve the enthesis at an early stage.
PIP in PsA and OA look similar on MRI
Historical studies of PsA PIP joint showed that enthesitis was very common [1]. MRI scanning of the PIP joint in early OA and PsA showed changes that were remarkably similar and it was often impossible to tell the two apart [2].
In both PIP OA and PsA, the most striking changes are evident in the entheseal attachment sites. [2].

|
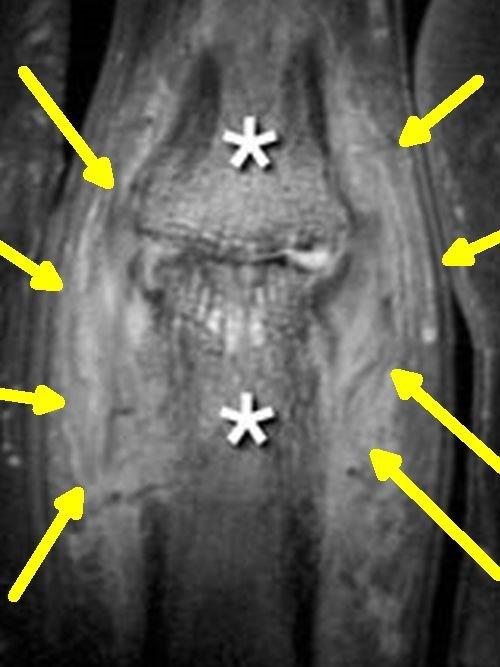
| This is an image of patient with a diagnosis of OA and it shows florid inflammation around the collateral ligament entheses of the joint (yellow arrows). This is associated with diffuse bone marrow oedema (white asterisks) |
The association between the enthesis and DIP disease in PsA is well established. [2]

|
| This image shows diffuse enthesitis of both collateral ligament entheses (yellow arrows) in a patient with joint swelling due to PsA |
Acute OA of PIP can be extremely severe
The degree of swelling of DIP joints in OA can be so severe that it mimics joint sepsis or severe PsA.
|
| This is a case with severe acute inflammatory OA with severe bone oedema (white asterisk) and lots of soft tissue inflammation involving the entheses (yellow arrows). The severity of inflammation associated with entheseal related pathology can be so severe that the doctors may mistake it as joint or bone infection. |
Implications
PIP joint swelling in a patient with psoriasis must be carefully considered to ascertain whether OA could be an alternative diagnosis.
Disease of the PIPs may be part of a more generalised pattern of arthritis which can help the physician establish the correct final diagnosis. At the present time, scanning of diseased joints is of limited value given that both PsA and OA attach the entheses.
Telling OA from PsA in the PIP
Disease of the adjacent DIP joints with nail involvement favour PsA
Look for dactylitis elsewhere in the body as this is characteristic of PsA
Swelling of the MCP joints (knuckles) makes PsA more likely.
Clear-cut swelling of an enthesis such as Achilles enthesis with bursitis makes PsA more likely
But remember both OA and PsA of the PIP joint can co-exist.
References

