Why don't all AS cases with Sacroilitis progress to spinal disease?
Introduction
Although the HLA-B27 gene is associated with the severity of bone inflammation in the sacroiliac joints, it is intriguing to note that it does not automatically tally with spinal inflammation which appears to be key for disease progression and spinal fusion.
The answer to this important question is not known and we only have theories on this page.
|
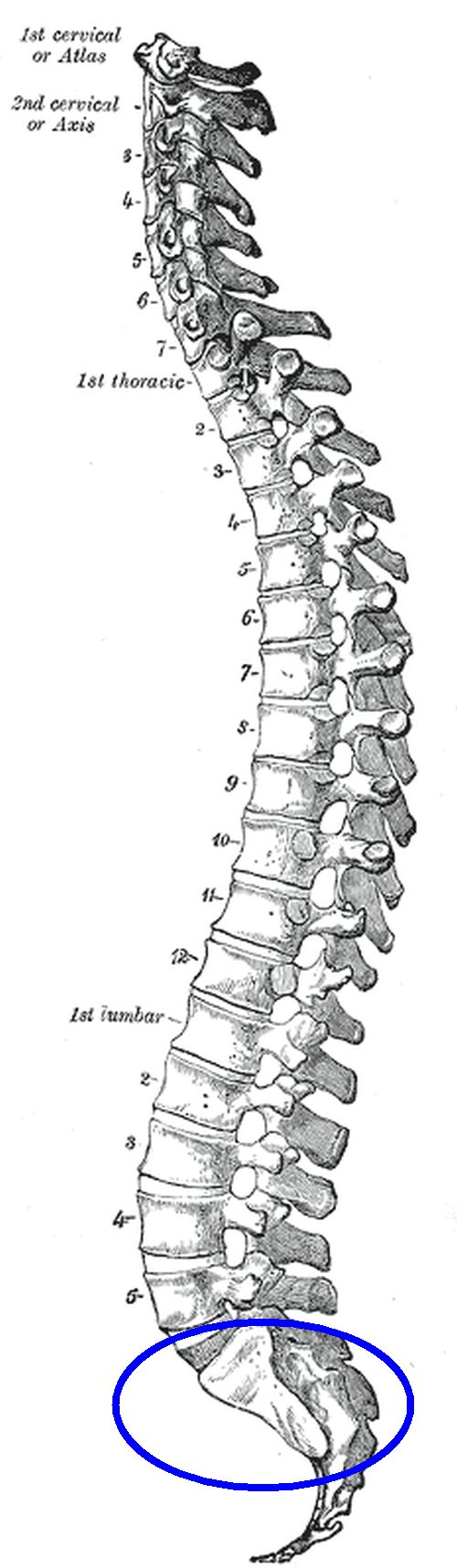
| This is the full length spine and sacroiliac joint component of the spine as viewed from the side (lateral view). The sacroiliac joint is inside the blue circle. Sacroiliitis is not necessarily associated with spinal involvement which is discussed on this page. |
Theories for non-progression of sacroiliitis to spinal inflammation
It is possible that some patients may be protected from potential pre disposing microdamage related entheseal lesions in the spine thus preventing the initiation of new lesions at that site. The available evidence from some occupations being more linked to disease progression supports the microdamage theory [1].
Immunomodulation or an ability to dampen down immune system T cell response could develop to lessen the inflammatory reaction following the initial sacroilitis. In the setting of chronic T cell immune activation against viruses, the T cells can become exhausted. Exhaustion of T cells, whose role remains to be proven beyond doubt in AS, is currently difficult to evaluate.
Another possibility is that inciting antigens such as in a Reactive arthritis are eventually cleared and the disease process burns out. According to this theory some people have a disease driven by a specific germ that once cleared leads to disease non-progression. In the case of Reactive arthritis, which can manifest as an AS type disease, studies have shown that clearing inciting bacteria with antibiotic therapy can switch off disease [2]. However, this has been shown for peripheral joints and not the spine.
An alternative explanation is down to differences in related gene expression in the spine and sacroiliac joint. There is no evidence for this so far.
It is likely that more than one mechanism may account for these differences.
References

