Misdiagnosis of Arthritis in Young People - The importance of Enthesitis
Undifferentiated Seronegative Spondyloarthropathy
Most types of potentially serious and treatable arthritis can often be recognised early.
For example, Rheumatoid Arthritis can typically be recognised in 70% or more of cases on the basis of small joint stiffness, swelling that may be subtle and a positive blood test called Anti-citrullinated protein antibodies (ACPA) or anti-cyclic citrullinated peptide antibodies (anti-CCP).
The second major category of inflammatory arthritis after Rheumatoid Arthritis is the Seronegative Spondyloarthropathies.
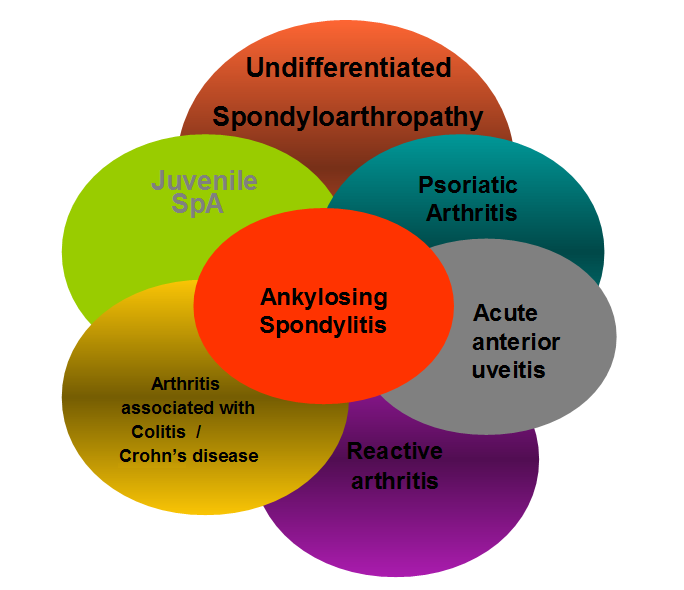 |
| Figure 1. Psoriatic Arthritis- A Unified Concept. Wright V. Arthritis Rheum 1978. The Seronegative Spondyloarthropathies comprise a group of clinically related conditions. As outlined below many of these can be recognised based on clinical and laboratory features but the poorly defined entity termed Undifferentiated Seronegative Spondyloarthropathy may be a particular reason for a delay in diagnosis. |
Why Undifferentiated SpA may go undiagnosed
Ankylosing Spondylitis is still not diagnosed quickly enough. However, low back pain, carriage of the HLA-B27 gene and a positive MRI strongly point towards that label.
Psoriatic Arthritis as a diagnosis is suggested by the presence of psoriasis which predates arthritis in about 70% of sufferers.
Reactive Arthritis is typically recognised by preceding infection within the previous month.
The presence of abdominal pain, diarrhoea, bleeding and other symptoms point towards colitis as being a cause of arthritis in a subgroup of Seronegative Spondyloarthropathy cases.
Uveitis can be used to diagnose a Seronegative Spondyloarthropathy type arthritis.
However, failure to recognise inflammatory pain, the absence of psoriasis or gut disease and absence of uveitis may lead to a complete failure to recognise Undifferentiated Seronegative Spondyloarthropathy. Such cases may have an absence of low back pain that is typical of Ankylosing Spondylitis and don't have the HLA-B27 genetic test performed.
This can be a major cause of a delayed or erroneous diagnosis.
It may take several years for the X-ray change of Spondyloarthropathy to develop, if they develop at all.
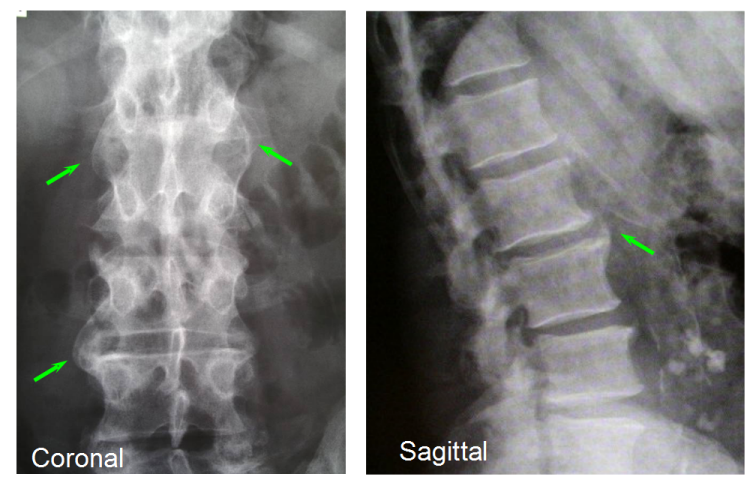 |
| Figure 2. X-ray changes of new bone formation at the enthesis in well established Spondyloarthropathy. Normal blood tests and normal X-rays near disease onset contribute to a delay in diagnosis. |
Illustrative Case
Boy aged 13 gets Achilles tendon pain playing football.
He is diagnosed as tendonitis- no response to therapy.
Subsequently diagnosed as Haglunds deformity and has surgery for both Achilles tendons regions.
Things settled for 3 months but eventually flared.
He subsequently developed knee pain and was diagnosed as Osgood-Schlatter disease.
He subsequently developed pain in the groin and was diagnosed as adductor tendonitis.
He failed to settle and was subsequently labelled as having a condition called Sports hernia.
A decade later he was diagnosed as having costochondritis.
At this stage he had several surgical procedures and still had no diagnosis.
He was referred to see a Rheumatologist.
He reported noctural pain, prolonged early morning joint stiffness, an improvement with exercise and an improvement with anti-inflammatory drugs.
By this time he reported a few bouts of wrist and knee swelling which was also documented by the consultant.
There was no psoriasis or family history of arthritis.
As he had been sexually active for several years the Consultant recommended that he get screened for Chamydia (a common cause of Reactive arthritis). This test proved negative.
His inflammatory markers were normal but he was positive for the HLA-B27 gene.
An X-ray of his low back was normal which fitted with the fact he did not report symptoms clearly referable to that site.
The diagnosis was Undifferentiated Seronegative Spondyloarthropathy.
He was then commenced on a treatment programme aimed at this inflammatory condition.
Learning points
Undifferentiated Seronegative Spondyloarthropathy is a diagnosis can easily be missed.
This patient picked up a series of enthesopathy related diagnoses including heel, knee and pelvic and chest involvement.
Although the original medical assessments defined the correct location of disease they failed to see that the problem was inflammatory rather than mechanical.
This resulted in unnecessary suffering and a delay in diagnosis.
Part of the problem is that mechanically related and inflammatory related enthesitis can look the same on MRI (the patient above did not have such scans).
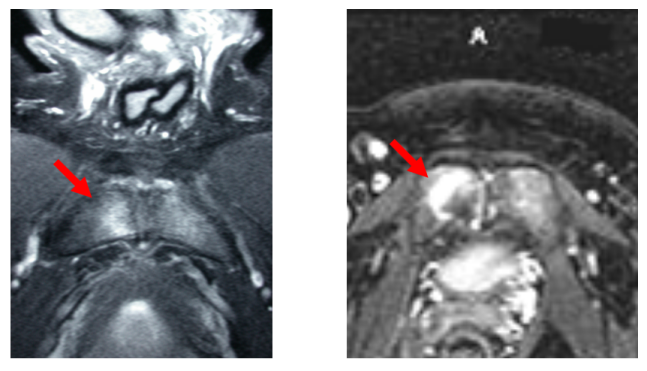 |
| Figure 3. The red arrow on the image on the left shows Magnetic Resonance Imaging determined "bone oedema" in the pubic bone region. The image on the right is from a patient with Spondyloarthropathy. Both look the same on scanning which can contribute to misdiagnosis. |
This website provides information relevant to the recognition of the enthesitis related arthropathy including Undifferentiated Seronegative Spondyloarthropathy.