Spinal Inflammation in AS
Introduction
The major cause of disability in long standing Ankylosing Spondylitis (AS) is spinal inflammation that may result in subsequent new bone formation. This page explains spinal inflammation in AS that is largely linked to enthesitis and adjacent osteitis and shows how spinal inflammation flip-flops from enthesis to enthesis.
What proportion of patients with early AS develop spinal inflammation?
The hallmark of AS is sacroiliac joint inflammation. However, it is recognised that only about half the cases with sacroiliitis on X-ray with a diagnosis of AS get spinal involvement. This figure is based on X-ray findings of spinal new bone formation in chronic AS.
Spinal inflammation in AS does not necessarily start after sacroiliac joint disease and gradually "spread up the spine" from the lower back, but may be patchy in nature and start anywhere in the spine.
In some people destined to develop AS, the initial pain may originate in the lumbar spine (low back) and be wrongly attributed to sacroiliitis. MRI scanning of the lower back in addition to the sacroiliac joint may help identify such cases [1].

|
| This is an MRI scan of the lumbar spine in a patient with inflammatory pain who is HLA-B27 positive. The sacroiliac joint was normal but the lower lumbar facet joint shows diffuse enthesitis (yellow arrows) |
Spinal Inflammation move around or flip-flop
Patients with AS may have chronic on-going spinal pain and stiffness that is typically associated with periodic flares in the disease. However, the exact location of enthesitis and associated osteitis may be moving around or "flip-flopping". This flip-flopping of inflammation also occurs in the sacroiliac joint and also in eye disease or uveitis in AS.
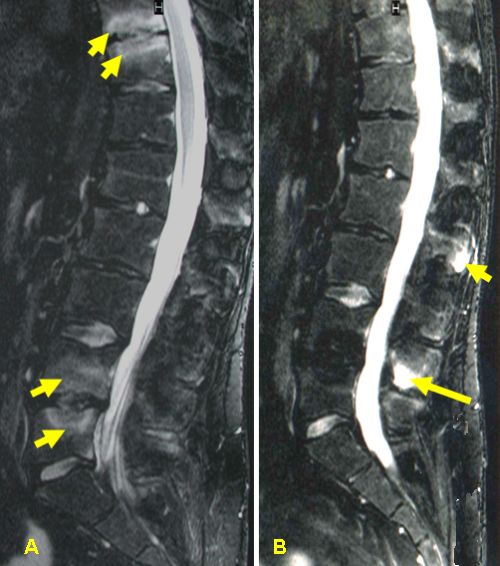
|
| The MRI scan marked A (left) was taken at baseline and shows lots of bone marrow inflammation or osteitis at the attachment site of the annulus fibrosus (yellow arrows). When the patient had a flare of disease and was rescanned on image marked B (right) the inflammatory lesions on the original scan had resolved. Now the patient had enthesitis of the interspinous ligament bony attachment site (yellow arrows). The pain is the same but the site is different |
Link between Inflammation and New Bone Formation
Not only is spinal inflammation painful but it is associated with subsequent new bone formation.
The HLA-B27 gene is also commonly linked with bony inflammation as seen MRI. About a third of HLA-B27 positive AS patients don't have bony inflammation on MRI at any given time (even when they have symptoms). [See spinal inflammation and Normal MRI in AS page] [2].
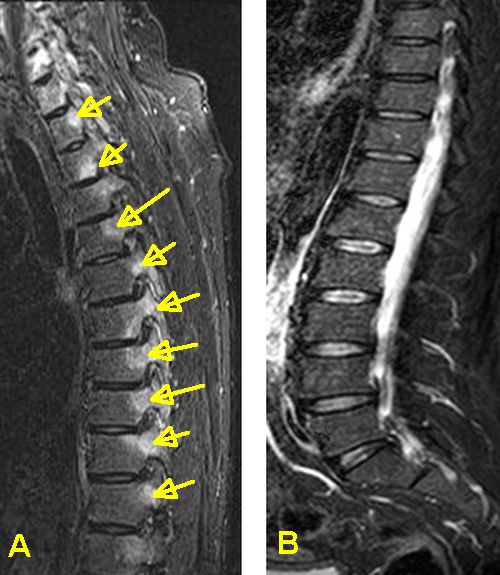
|
| MRI scan A and MRI scan B are from patients with a similar levels of back pain and stiffness. However, only MRI scan A (left) is abnormal with multiple enthesitis and associated osteitis areas of inflammation (yellow circles). A normal MRI does not exclude low level enthesitis including inflammation of the soft tissue component of the enthesis. |
There is a link between spinal inflammation as measured by C-reactive protein (a blood marker of inflammation) and subsequent new bone formation [2]. However this marker is not elevated in many cases of AS with spinal inflammation.
A positive MRI scan has also been linked to new bone formation on X-ray in AS. But cases with normal MRI scans may also progress
Spinal enthesitis as detected by MRI is associated with a better response to biological therapies in AS.
Implications
In general, the absence of detectable MRI changes in the spine in AS may be associated with a lower risk of progression to bone fusion. Determining which patients are likely to have spinal inflammation may be key to ensuring that the highest risk patients get treatment.
However, patients without spinal MRI inflammation, who may be less likely to progress to new bone formation, may derive benefit from biological therapy. This has lead to the debate around using these biological agents as "expensive painkillers". Research is on-going in this area.
References



Resources
American College of Rheumatology Spondylarthritis (Spondylarthropathy)
Lab Tests Online - Information on C-reactive protein (CRP) and inflammation testing