The Two Types of Enthesis
Two types of insertion exist - fibrocartilagenous in nature (these are abundant) and fibrous in nature (these are relatively uncommon).
The fibrocartilagenous enthesis is most strongly associated with disease states including ankylosing spondylitis and psoriatic arthritis.
The Fibrocartilagenous Enthesis
The pulling action along the tendon/ligament creates what is called a shearing force at the insertion.
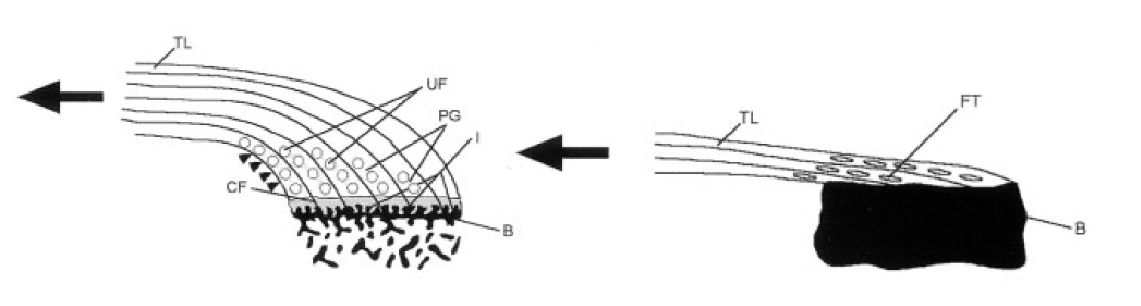
The tendon or ligament of the fibrocartilageous enthesis is kinked because it is inserted close to the joint space (see figure).
The resulting change of angle of the tendon or ligament adjacent to the joint creates pressure on the deeper layer of the enthesis.
The matrix produced by the fibrocartilage cells at such locations is called glysocaminoglycan or proteoglycan and resists stress (see figure).
This anatomical arrangement and complex forces with both shearing and compression is what actually leads to the fibrocartilage formation at the enthesis (see figure).
p>The magnitude of forces acting at the enthesis directly dictates the thickness of shock absorbing fibrocartilage at a given site.The Fibrous Enthesis
In contrast, the fibrous enthesis is inserted at a considerable distance from the joint and there are virtually no compressive forces because the tendon or ligament is not kinked.
The mechanical forces acting on this type of enthesis are less complex, there is no fibrocartilage and disease states are less common.
Fibrous entheses are inserted into the midshaft of long bones.
The fibrous enthesis may attach directly to the bone.
The fibrous enthesis may insert directly into the surface layer of the bone termed the periostium.
The skeleton of a child or young person has a thick periostium that regresses with age so the nature of a fibrous enthesis insertion may change with age.
The fibrous enthesis may have fibres of collagen from the tendon or ligament directly entering the calcified part of the bone. These are called Sharpeys fibres.
The fibrous enthesis being attached to thick bone cortex is not associated with diffuse inflammation in the underlying bone cavity.
 |
|
| TL = tendons or ligaments. I = microscopically irrelgular interface between enthesis and bone. CF = calcified fibrocartilage or hard bone enthesis junction. B = bone. UF= uncalcified fibrocartilage at enthesis bone interface, this is compressible. PG = proteoglycan which is the shock absorbing material made by fibrochondrocyte cells at insertion. FT = dense fibrous tissue. The arrows show the direction of pull. The arrow heads show the sites of maximal compression that is key for fibro cartilage formation. | |
Implications of the two types of enthesis
In reality many fibrocartilageous entheses also have a fibrous component. This is usually located on the outside edge of the insertion.
Since fibrocartilage develops naturally at sites of shearing and compression, a surgeon does not need to worry about implanting this tissue during tendon or ligament repairs. If the procedure recreates the correct mechanics then the fibrocartilage tissue should develop from the ends of implanted tissues.
Sharpey's fibres have enjoyed a lot of publicity in the past. However, these are absent in the insertions most typically affected by ankylosing spondylitis, psoriatic arthritis and the allied disorders and are not key factors in disease.