Lupus and Entheseal Joint Pain - Is there a link?
The case history
The patient was a 36 year old lady.
Her mother had lupus and was on treatment.
The patient went to bed feeling generally unwell.
She woke up the next morning with a painful and swollen left knee.
She simultaneously developed flu like symptoms with throat discomfort that persisted for two weeks.
She also developed elbow pain and stiffness.
Examination findings
There was tenderness at the triceps tendon insertion.
The knee joint swelling had resolved.
The patient had persistent patellar tendon origin and insertion enthesitis.
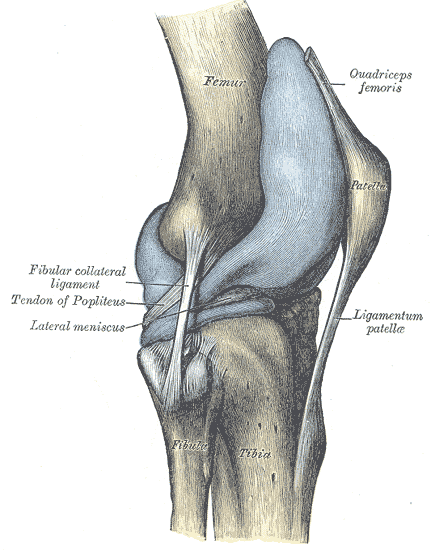 |
| There was tenderness over both ends of the ligamentum patellae. |
She also had peroneal tendon synovitis on the right ankle.
Results of Investigations
Her inflammatory makers were normal.
She did not carry the HLA-B27 gene.
Here Anti-Nuclear Antibody (ANA) was homogenous with a value of 1/160 (normal is less than 40). Her Extractable Nuclear Antigen was negative.
Her other immunological related blood tests were normal.
Working diagnosis. Her primary physician made a diagnosis of lupus that was presenting with arthritis.
Questions and Lessons
What is the cause of joint pain in this case?
What is the diagnosis?
Is it lupus or Reactive Arthritis?
The referring doctor considered that the patient had SLE like her mother. However there is a high prevalence of ANA positivity in first degree relatives of patients with lupus which may have been the case in the patient above. The patient had no other features of lupus and an extensive array of normal blood tests.
The patient had clear cut enthesitis at 3 sites. Peroneal tenosynovitis is part of what is termed as functional enthesis inflammation where tendons wrap around bones. This is a common site of inflammation in Spondyloarthropathy (SpA). However, tendon inflammation is also common in lupus.
The overall pattern of disease fitted better with a Reactive Arthritis even though there was not a clear cut history of infection that predated the arthritis. However, the flu symptoms and polyenthesitis and isolated transient knee swelling were most compatible with this diagnosis.
Reactive Arthritis is a reaction to an infection in another part of the body but living germs are not present in the inflamed joint tissues. It commonly manifests as enthesitis.
The working diagnosis was therefore an Undifferentiated SpA or a related Reactive Arthritis. The HLA-B27 negative status was taken as a good prognostic sign. The patient was given intra-muscular depomedareon 120mgs.
Lupus and Joint pain due to Enthesitis at multiple sites
There is very little evidence in the literature suggesting that enthesitis is common in SLE.
Rare case reports might represent dual pathology or a misdiagnosis of lupus as in this case.
Making a correct diagnosis is important as Reactive Arthritis often runs a benign course where lupus is more likely to be chronic.