Bone Erosion in Ankylosing Spondylitis
Introduction
Bone erosion is a process whereby the surface of a bone (the bone cortex) is degraded or eroded and is most typically seen in the setting of inflammation. In this context specialised cells termed osteoclasts dissolve the bone surface. Erosions related to disease seem to correspond to microscopic erosions at sites of microtrauma adjacent to entheses in the normal non-diseased skeleton. This page explains mechanisms of spinal erosion in Ankylosing Spondylitis.
Bone erosion in Ankylosing Spondylitis may occur in the peripheral skeleton, for example, in a swollen knee. Such erosion formation may also occur at peripheral entheses. The purpose of this article is to review bone erosion and its significance with an emphasis on spinal disease in Ankylosing Spondylitis.
Terminology Difficulties
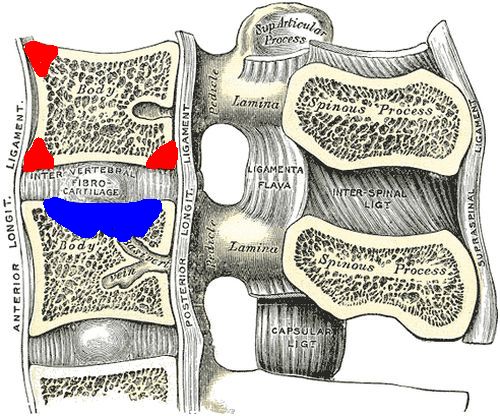
The discs of the spine that join vertebrae together are elaborate entheses. Depending on where putative initial microdamage takes place different names are given to the enthesis related erosions. The two types of spinal bone erosion in Ankylosing Spondylitis termed Anderson and Romanus lesions are shown below [1,2].
|
| Common sites of Erosion related to the insertion of the discs to vertebrae. Red = corner erosions that are called Romanus lesions. These may be associated with a bone repair reaction on X-ray that is termed a shiny corner. Blue= Anderson lesion. This is a type of erosion of the bone likely related to a "blow out" of the central soft part of the disc called the nucleus pulposis. |
These types of erosions were originally described on X-ray and more recently have been describe on MRI. However, since MRI lesions may not necessarily be associated with discernible bone cortex destruction and some researchers feel that it is wrong to use such terminology for MRI damage [3].
Site of spinal erosion in AS
Erosions in the spine in early Ankylosing Spondylitis typically occur at the anterior enthesis insertions of the vertebral bodies. We believe that they are at least in part linked to microtrauma at the enthesis insertion to bone. This is because tissue from normal spines in subjects without Ankylosing Spondylitis show microscopic damage or micro-erosions at the same anatomical site where erosions in Ankylosing Spondylitis typically occur [4].
In Ankylosing Spondylitis these corner erosions trigger a florid inflammatory reaction in the adjacent bone on MRI. This bone reaction is linked to carriage of the HLA-B27 gene.
Unlike the erosions in rheumatoid arthritis the erosions in the spine in Ankylosing Spondyliits appear to repair with time. When X-rays are performed the erosion may already be repaired and what is visible is a "shiny corner" due to the adjacent bone reaction. Indeed over-repair with actual fusion of the adjacent entheses and segmental fusion of the spine may occur.
The central type erosions or Anderson lesions may occur in early Ankylosing Spondylitis and are directly related to inflammation. Such lesions in advanced Ankylosing Spondylitis may be due to trauma and fracture through the fused disc enthesis with the treatment being very different [5].
Spontaneous healing of Bone Erosion in AS
Bone erosion in the peripheral entheses in Ankylosing Spondylitis and Spondyloarthropathy appears to repair over time [6]. Such erosions are linked to CRP levels and entheseal Doppler signals on Ultrasound examination. This confirms the key role of inflammation in erosions in Spondyloarthropathy.
As a result bone erosion was noted to be commoner in early Ankylosing Spondylitis and Spondyloarthropathy compared to late disease.
Bone Erosion at other sites in AS
Bone Erosion in the sacroiliac joint in also a feature of Ankylosing Spondylitis. The sacroiliac joint is characterised by widening and erosion in early disease. With time these erosions also fill in and are followed by subsequent fusion of the joint with loss of movement.
Implications of spinal erosion in AS
The biggest problem for a patient with Ankylosing Spodylitis is that these erosions may be misdiagnosed as a septic discitis or osteomyelitis. This could lead to unnecessary tests and investigations. A close interaction between alert physicians and dedicated musculoskeletal radiologists is needed to hasten an early accurate diagnosis.
Erosions and associated bone marrow oedema reactions as determined by MRI may paradoxically be an early predictor of future spinal fusion. However, MRI determined inflammation on its own without visible erosion also may predict spinal fusion [7]. This is because inflammation at the enthesis-bone junction is the forerunner of large imaging evident erosion. So inflammation as readily visualised on MRI scanning is a good predictor of the erosion related pathological process.
To summarise, entheseal related erosions are common in Ankylosing Spondylitis and in keeping with the reparative nature of this condition these usually repair with time, irrespective of therapy and are also associated with excessive new bone formation.
References





Resources
Medscape Imaging in Ankylosing Spondylitis