SAPHO syndrome and Enthesitis
Introduction
The SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome is a type of arthritis that typically involves the sternoclavicular joint and is an uncommon manifestation of Psoriatic Arthritis (PsA) and the related Spondyloarthropathies (SpA). This page explains the biomechanical link between the SAPHO syndrome and diseases of the enthesis.
SAPHO and Enthesitis
The sternoclavicular joint is a firbocartilagenous joint and this type of joint is a particular target in PsA and SpA due to its biomechanical properties.
The SAPHO syndrome has being linked to enthesitis on X-rays of the sternoclavicular region where damage at attachment sites is evident [1]. Also patients with SAPHO syndrome of the sternoclavicular joint often have painless enthesopathy as determined by ultrasound at sites remote from the lesions [2].
Disease Mechanism in SAPHO
Bone adjacent to fibrocartilage experiences both compressive and shear forces and this is linked to diffuse bone inflammation which is known as osteitis. This osteitis may trigger bone destruction with the bone being re-absorbed (termed osteolysis). The osteitis may also stimulate bone stem cells on the bone surface resulting in excessive new bone formation (hyperostosis).
SAPHO is typically associated with acne like lesions with pustules on the soles of the feet and palms of the hands but these are not universally present. Patients may also have severe acne at other locations.
Tissue studies
The acute inflammatory phase of SAPHO in both the skin and joints is associated with infiltration of inflammatory cells called neutrophils. These cells are the "first line of defence" and are part of the innate immune system. This suggests that the SAPHO syndrome is "autoinflammatory" or driven by innate immunity. The generally good long term prognosis also suggests that innate immunity rather than autoimmunity is dominant in SAPHO [3]
Diagnosis
Painful swelling and tenderness of the breastbone and collar bone junction region is evident.
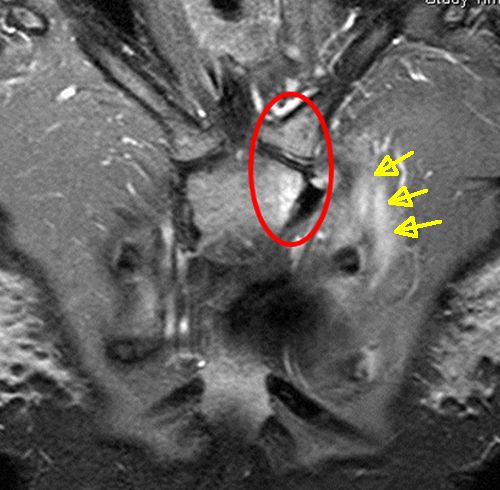
Magnetic Resonance Imaging (MRI) studies in early disease show severe bone oedema (due to inflammation) without bone cortex destruction.
|
| This is a fat suppression MRI scan showing SAPHO of the left collar bone and adjacent breastbone (clavicle) in a patient with Psoriatic Arthritis. The white region inside the red circle is the bone marrow inflammation which is called bone oedema on MRI. The yellow arrows show soft tissue inflammation outside the joint. There is no tissue destruction or collections which is typical of early SAPHO. |
Other tests including X-rays and ultrasound scanning of the joint can be performed. Fluid may be aspirated under ultrasound guidance from the joint cavity where visible.
Before the advent of MRI and in an era when SAPHO was less well recognised open surgical biopsies were often performed. In the modern era, in the proper clinical context and with an MRI scan showing no cortical destruction and in the presence of psoriasis or acne, many doctors would make a clinical diagnosis. Liaison between Rheumatologists and musculoskeletal radiologists is advisable. In patients with SAPHO syndrome, MRI scanning of a wider area may show silent bone abnormalities at other entheses.
When in doubt an open biopsy may be need to exclude other pathologies such as infection or cancer.
Pitfalls
When SAPHO occurs in other fibrocartilagenous joints such as the acromioclavicular joint it may be poorly recognised and have a delayed diagnosis [4]. The condition may present acutely to hospital and be initially be given the wrong diagnosis of joint infection of osteomyelitis.
SAPHO has been also described in the jaw (temperomandibular joint) which is another firbocartilagenous joint [5]. Typically disease at this site may manifest as infection or even a tumour due to tissue destruction.
Treatment strategies
In many cases the disease may run a self-limiting course
After a correct diagnosis has been made local or systemic steroids have been used.
Antibiotics have been used but without great effect.
Bisphosphonates may certainly inhibit the bone remodelling and destruction.
Agents including methotrexate and sulphasalasine are not proven.
The anti-TNF class of drugs appear to be effective.
References





Resources
Medscape: Acne Fulminans A good review on severe acne and SAPHO
MedicineNet.com SAPHO Syndrome