The Hip in Ankylosing Spondylitis
Introduction
After sacroiliac and spinal involvement the next most common joints to be afflicted in AS are the large joints including the hips. Hip disease can be difficult to recognise because the joint is located deep to several large muscles. Hip disease can be hard to tell apart from sacroiliitis and inflammation at both sites can also co-exist. Hip disease can rapidly progress to joint destruction. Although no formal studies have been performed, it appears that early recognition and prompt therapy may save the hip joint from severe damage in AS patients.
Symptoms of hip Disease in AS
Pain may be felt in the groin and localise fairly well to the hip region.
Pain may be felt in the buttock region and can mimic sacroiliitis.
Pain may radiate down the leg to the knee.
Early morning stiffness.
Examination
Limping may be evident.
Global restriction of hip movement should raise awareness of potential hip involvement.
In some cases hip pain is due to trochanteric bursitis due to inflammation at buttock muscle entheses which manifests as tenderness over the bone and not being able to sleep on the affected side.
Severe sacroiliac joint inflammation in a patient without hip disease may lead to hip movement restriction thus confusing the exact diagnosis.
Diagnosis
In early AS related hip disease X-rays are usually normal.
In the modern era the doctor should request an MRI scan of the entire pelvis to include hips and sacroiliac joints rather than scanning the sacroiliac joint alone.
In a young person presenting with hip disease and absent back pain with early AS there is a good chance that the diagnosis could be completely missed.
The biggest cause of confusion is septic arthritis or osteomyelitis.
If MRI shows clear-cut sacroiliitis in addition to hip disease then AS hip involvement is likely and open biopsy should not be necessary.
Ultrasound of the hip with aspiration of fluid from the joint cavity to exclude infection may be carried out. In a subject who carries the HLA-b27 gene and showing sacroiliitis on MRI scanning this may not be necessary.
Patients with isolated early hip disease may have open biopsy performed to exclude other pathologies.
|
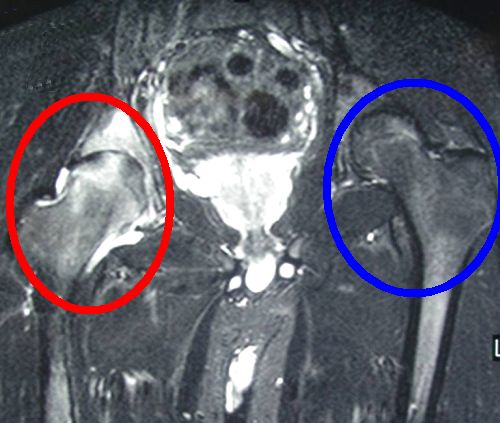
| This is an MRI scan of severe right hip involvement in AS. There is high signal which is white inside the red circle indicating in this case severe inflammation. The left hip (blue circle) is normal. The MRI must be interpreted in the context of the history, examination and blood tests. |
Careful consideration between experts including rheumatologists, radiologists and orthopaedic specialists may minimise the need for hip drainage or biopsy
Treatment
For early hip disease corticosteroids may help, at least as a short term measure. These can be injected into the joint, injected intramuscularly or as taken as tablets.
Conventional disease modifying anti-rheumatic drugs have no proven role. However, they may be used since biological therapies generally don't have a licence for isolated hip disease.
The anti-TNF agents appear to be very effective for hip involvement in AS but there is little direct information. The anti-TNF agents when used for spinal disease appear to protect against hip disease progression in AS [1].
References

Resources
See Hip Tendonitis and Bursitis Differential Diagnoses for a more detailed list of other possible causes of hip pain.