Foot and Ankle in PsA
Introduction
Ankle and foot involvement may be part of a generalised form of PsA or may occasionally be the only manifestation of PsA. It is an important problem that deserves careful attention [1,2]. This page explains the link between enthesitis and ankle and foot disease.
Entheses in the Foot and Ankle
There are 26 bones in the foot. These have multiple capsular entheses and associated stabilising ligaments. There are over 20 muscles in each foot many of which have multiple attachment sites.
Inflammation or large entheses such as the Achilles is easy to recognise but enthesitis at other large entheses is less well recognised. There are many small and inaccessible entheses where the clinical recognition of inflammation is virtually impossible to define.
Functional Enthesis or wrap around tendon pain
There are several regions of wrap around tendons or "functional enthesis" in the ankle joint and midfoot. Patients may also experience pain and inflammation at these sites which is poorly recognised.
|
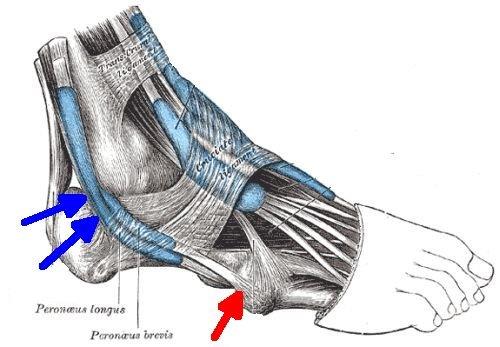
| This image shows the location where the peroneus brevis and longus tendons wrap around the fibula which acts as a bony pulley on the outside of the ankle joint (blue arrows). This structure functions like an enthesis and may lead to pain and inflammation in PsA. The peroneus brevis attachment site is shown in red. |
Enthesitis of the peroneus brevis insertion which manifests as pain on the outside of the foot is not well recognised but may respond to a local injection. The blue arrow on the image above shows this enthesis.
On the opposite side of the ankle the tibialis posterior tendon functional entheses may also be subject to inflammation. Disease of these wrap around tendons typically manifests as soft tissue swelling or tendonitis but it has the same underlying mechanism as enthesitis.
|
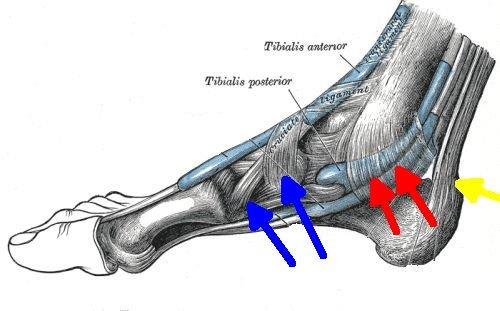
| This image shows the tibialis posterior tendon functional enthesis may also be subject to inflammation (red arrows). Disease of these wrap around tendons typically manifests as soft tissue swelling or tendonitis but it has the same underlying mechanism as enthesitis. The blue arrows show the tibialis anterior enthesis. The yellow arrow shows the Achilles enthesis which is relatively well recognised as a cause of pain because of its large size. |
Tibialis anterior enthesitis may manifest as ankle pain and swelling on the inside of the foot. Inflammation of this enthesis is not well recognised by doctors which is complicated by the fact the tendon has two distinct insertions.
Enthesitis of the small intrinsic muscles of the foot or the small ligaments in the foot is much harder to recognise. It may also manifest as soft tissue swelling or bone pain.
Diffuse bone marrow inflammation in the foot
The biomechanics of the joints in the midfoot which are lined by fibrocartilage is similar to that of the enthesis. One or all of these structures can be diseased in PsA.
Diffuse bone inflammation or osteitis may also be seen and manifest as soft tissue swelling.
|
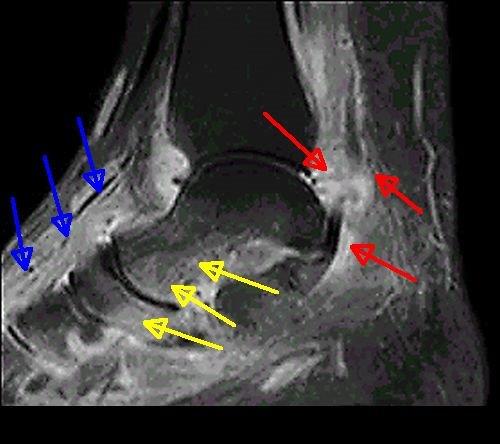
| This image shows PsA of the ankle and foot in a 32 year old man with psoriasis. The MRI scan shows diffuse swelling and inflammation of all the tissues. The red arrows show inflammation at the "functional enthesis" where the tendon wraps around the bone. The yellow arrows show diffuse bone marrow inflammation (osteitis) which occurs adjacent to fibrocartilage which is present in the joints of the midfoot. The blue arrows show diffuse inflammation of the soft tissues on top of the foot. This pattern of soft tissue swelling may be linked to bone inflammation (osteitis) that triggers a reaction on the bone surface (periostium). |
Diagnosis of PsA foot disease
This is usually made on clinical grounds but scanning may help.
Psoriasis subjects are especially prone to dactylitis or sausage toes which is common in the feet. It may not cause pain so it is important to check the toes carefully.
Diffuse bone inflammation on MRI may be misdiagnosed as a bone infection (osteomyelitis) which could lead to prolonged antibiotic therapy that will make no difference. Another potential incorrect diagnosis is bone stressing or bone bruising.
Treatment of foot disease in PsA
Firstly, it is important to confirm that the foot pain is due to inflammatory enthesitis rather than mechanical enthesopathy. Identification of mechanical factors that could be driving or exacerbating inflammatory disease including flat feet (pes planus). Specialised input from a podiatrist may be very useful, even if the pain is primarily coming from inflammation in the foot, because the other issues can also be addressed.
Footwear should be assessed with insole provision if needed.
Weight loss may also be advisable as many PsA patients are overweight
Analgesia strategies including paracetamol or codeine are not generally very effective but may help some patients.
Non-steroidal anti-inflammatory strategies may help.
Corticosteroid injection may be used and depending on the site of enthesitis may be injected adjacent to the inflamed enthesis (for Achilles) or directly into it (for plantar fascia).
If the enthesitis is very disabling then more potent disease modifying or biological drugs could be considered. However, in the UK and other countries these are not licensed for isolated disabling foot enthesitis and a special case for their use in this setting would need to be made. The literature in the past 3 decades shows how therapy for resistant enthesitis including foot enthesitis has dramatically improved, especially since the arrival of biological drugs.
References

