Osteitis in AS
Introduction
Osteitis means bone inflammation. The pain from sacroiliitis in Ankylosing Spondylitis (AS) is often due to osteitis. However, osteitis can occur at multiple other sites in AS. This page explains the importance of osteitis as an unrecognised cause of pain in AS and shows examples from different locations.
Importance of Osteitis in AS
The osteitis pain is often severe and since it is coming from the bone, it may be deep seated and hard for doctors to properly recognise. This may contribute to a delay in diagnosis of AS or Spondyloarthropathy. It may also be misdiagnosed as septic arthritis or bone infection (osteomyelitis).
Link between Osteitis and Enthesitis
The fibrocartilagenous entheses are anchored to the bone like the roots of a tree to the ground hence the link between the enthesis and bone. Several joints prone to AS are also lined by fibrocartilage. The complex bone stressing adjacent to fibrocartilage appears to play a role in the development of osteitis at seemingly diverse sites. This unified basis for osteitis in AS is reviewed in section on Enthesis Anatomy and Physiology.
It is known that the MRI changes are due to osteitis since biopsy studies have confirmed the presence of immune cell infiltration at these sites [1].
This page illustrates that the pattern of osteitis in AS but these are also seen in the other Spondyloarthropathies.
Examples of Osteitis in AS
Sacroiliac Joint
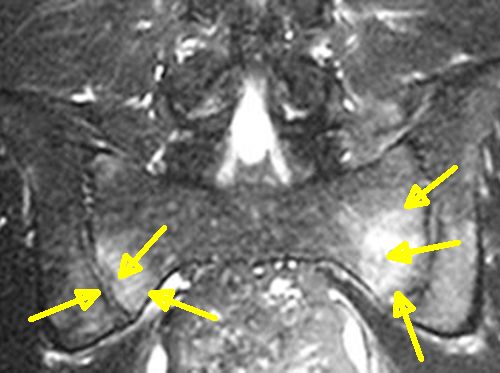
|
| The yellow arrows show the diffuse osteitis (white) in both sides of the sacroiliac joint |
Diffuse osteitis of the sacroiliac joint and spine and its persistence is linked to the HLA-B27 gene
Spine

|
| The yellow arrow shows diffuse vertebral body osteitis in a patient with AS. On its own this could indicate other pathologies including infection or tumours or trauma. However, the focal area of osteitis at the anulus (yellow arrow) is typical of AS and Spondyloarthropathy. This less severe lesion helps confirm the diagnosis. |
Large Joints- example of knee
Diffuse peri-enthesal osteitis is less common in the knee compared to the spine. This severe pattern of bone pathology is only present in a subset of cases.
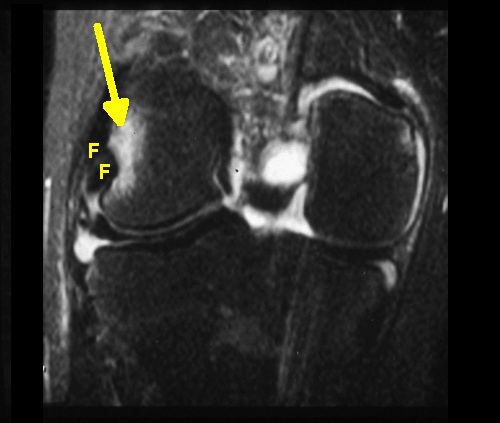
|
| The yellow area shows osteitis adjacent to the collateral ligament of the knee in a patient with AS. F= fibrocartilage which appears black since it appears non-inflamed since it lacks a blood supply. |
Heel Disease
This is plantar fasciitis in a patient with AS. There is extensive and unexpected osteitis in the underlying calcaneus.
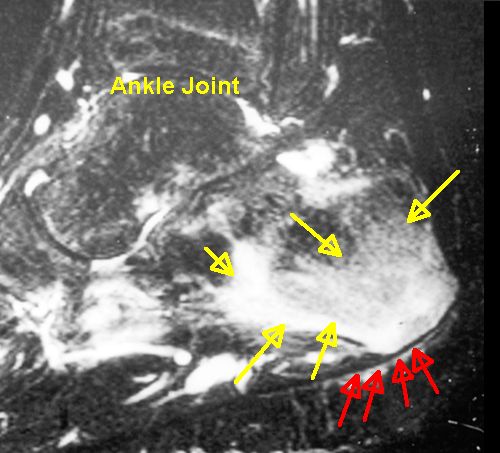
|
| This HLA-B27 positive case has severe plantar fasciitis and bone pain. The yellow arrows show severe osteitis adjacent to the plantar fascia attachment site (red) |
Wrap around tendons
Where the tendons wrap around bony pulleys as in the foot there is extensive bone inflammation. Such "wrap around tendons" which are termed "functional entheses" as they have fibrocartilage at the point of bone compression. We believe that this may trigger subsequent bone surface inflammation termed periostitis.
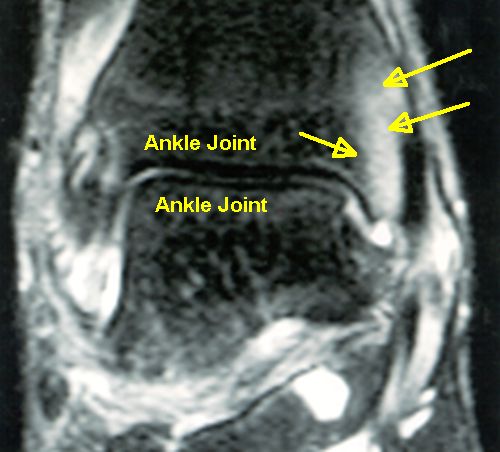
|
| This scan shows diffuse osteitis underneath the fibrocartilage of the compressing tibialis posterior tendon. |
Breastbone
This is the SAPHO syndrome where there is extensive bone inflammation adjacent to the entheses and the fibrocartilagenous joints in this HLA-B27 positive case.
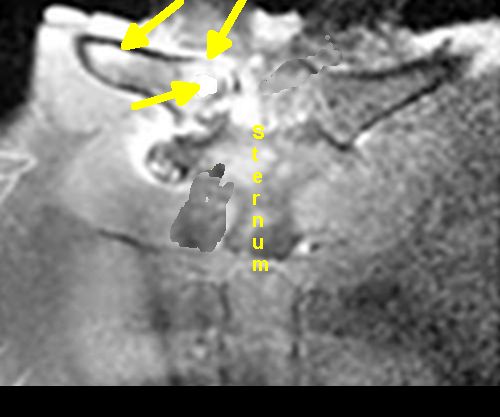
|
| This scan of the breastbone (sternum) shows severe osteitis. This occasionally occurs in HLA-B27 positive cases. |
Pubic Symphysis osteitis
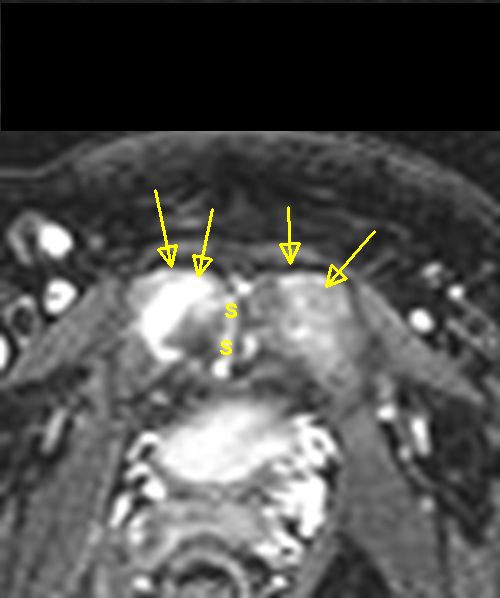
|
| This scan shows severe osteitis (in yellow) over the pubic bone in a patient who had difficulty walking. S = symphysis fibrocartilagenous joint |
Hip Osteitis
It is important to recognise hip osteitis in early AS and SpA as it may be the initial disease manifestation and be associated with a bad prognosis.
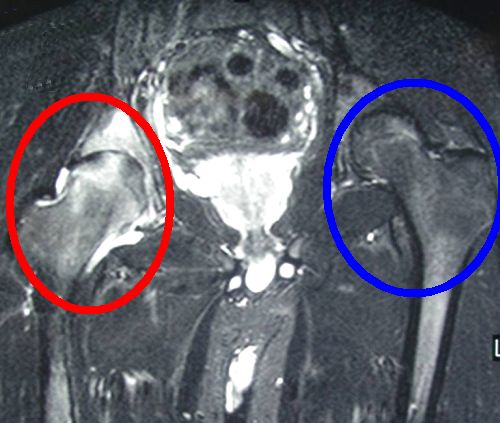
|
| This MRI scan shows severe osteitis in the right hip (red circle) compared to the normal unaffected left hip (blue circle) |
Implications
Osteitis can be extremely painful but may not be associated with obvious swelling.
Timely recognition of osteitis related pathology in AS is important to minimise pain and suffering, unnecessary tests and treatment.
The osteitis lesion is remarkably sensitive to therapy with the anti-TNF agents. More data is needed on newer agents.
References

Resources
Differential diagnosis for sacroiliac joint disease. This site offers alternative considerations in a patient with changes compatible with osteitis on MRI.